Polyvagal Theory
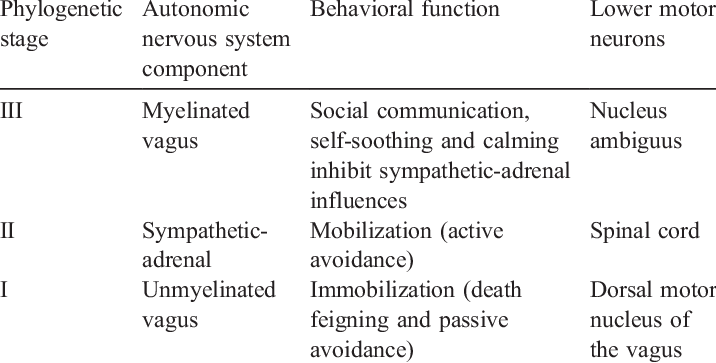
In the first article in this series (read here if you missed it!), we got an overview of the vagus nerve and its role in stress physiology. In this second article, we will go through the specific stages of the stress response in polyvagal theory. These stages, in order from least to most evolved, are the unmyelinated vagus, the sympathetic-adrenal system, and the myelinated vagus (Table 1).1 By most evolved, I mean that only the unmyelinated vagus is present in different reptiles, amphibians, and primitive vertebrates. Over time, animals evolved to develop more effective means and physiology to cope with stressors.
These stages rely on a balance between excitation and inhibition—essentially when one stage is activated, the other stages are turned off. For everyday stressors (work deadlines, conflicts with partners, too much homework, election results, etc.) we tend to rely on the most evolved stage (the myelinated vagus) and suppress the other two. When the stress we experience becomes too great, we go down to the next, more primitive stage. Let’s go through each stage one by one, starting with the least evolved, and thus the simplest, stage.
Stage I: Unmyelinated Vagus
The most primitive stage, immobilization, can occur when the unmyelinated vagus is activated. Immobilization typically refers to feigning death in animals and fainting for humans. It focuses on conserving resources, most notably by maintaining low heart rates, also known as bradycardia. It can be adaptive for reptiles and some other animals to feign death, but mammals require more oxygen and thus can experience severe damage from entering this stage.1 In these videos, you can see a shark in ‘shark trance’ and a snake experiencing tonic immobility, two forms of this vagal response. This mechanism is not always the most effective, which is why mammals did not evolve to utilize it, as shown by this video in which an alligator is temporarily placed into such a state.
You won’t engage this stage in your daily life—this stage only occurs in cases of extreme stress in humans. People who chronically experience this stress response are diagnosed with vasovagal syncope, which you may have heard referenced in TV shows like Scrubs and America’s Next Top Model. People with this condition faint in response to either situational triggers, intense stress or emotional triggers (e.g., seeing blood), or from standing for too long. The exact mechanism of this disorder is unknown, but experiments in cats suggest that vasovagal syncope is caused by sudden activation of the unmyelinated vagus.2 This can be a life-long condition, or may be seen temporarily in someone experiencing a high amount of stress.
Stage II: Sympathetic-Adrenal System
The sympathetic-adrenal system is the second stage of the system. It mobilizes the fight-or-flight system in the body, as described in the previous article, when a threat is detected (You can see this process in action as an iguana runs for its life from predators). The sympathetic-adrenal system requires a lot of energy, and we therefore only engage this system when the environment is considered unsafe. How do we know to activate this system then? According to Porges, we are subconsciously evaluating our environments via the process of neuroception; we are constantly evaluating our own safety and whether the environment poses a threat1.
Let’s compare sensation, perception, and neuroception. Sensation refers to when we receive sensory inputs and is entirely physiological, whereas perception refers to how we interpret these sensations (e.g., the blue-black gold-white dress fiasco). Everyone was looking at the same picture, so their eyes were experiencing the same sensory input, but people perceived the dress differently. Neuroception doesn’t fall neatly into either of these categories. It refers to how we distinguish between a threatening situation and a non-threatening situation—if you get into a fight with someone, you may not necessarily think “this is a threatening situation” but you your brain can interpret contextual cues and stimuli (e.g., the facial expressions, appearance, vocal tone, etc.) to determine that there is a threat. Thus neuroception is not only the perception of stimuli, but the assessment of whether the environment is safe or not based on these stimuli. Evolutionarily this system is favorable because animals can escape when they perceive a predator nearby.
This response clearly promotes survival from physical danger (e.g., snakes!), but it can also activate in response to psychological stressors. For example, imagine that while talking to that special someone you are trying to impress, your friend decides to tell an embarrassing story about you. You might try to act calm, but your face betrays you by turning red, your heartbeat increases, and your palms start to sweat. These physiological responses are mediated by the sympathetic-adrenal system.3 Your body has detected an emotional threat and is reacting as if there were a physical threat. Thus, this pathway – while advantageous for an animal in the wild—is not the most adaptive for social interactions and daily functioning in society.
Stage III: Social Engagement System
The integrated pathway that enables us to interact daily with the environment is termed the Social Engagement System. This system controls the regulation of the striated muscles of the head and face, as well as the myelinated vagus’ regulation of visceral organs.1 The system works two-fold by 1) regulating our psychological distance from threats and 2) filtering stimuli and engagement with others.5 For example, when babies see their mother, they may feel more secure. Their social engagement system may reduce psychological distance by vocalizing to the mother and listening to her voice. The baby may increase engagement by keeping its eyes open and to orient toward the mother. By controlling the face, this system is involved in expressing emotions, as well as looking at and hearing others. This system of neural circuitry incorporates a variety of cranial nerves, each serving a unique function.
These neural circuits begin in the cortex. Again, we are continually scanning our environment for threats via neuroception. We enter Stage 2, the sympathetic-adrenal system, when a threat is detected. When a threat is not detected and we feel secure, the social engagement system is activated; the stress response is inhibited and the cranial nerves are activated to promote engagement. The myelinated vagus is just one of a series of cranial nerves involved in this response.
It is important to note that animals originally had only an unmyelinated vagus involved in parasympathetic activity. Mammals evolved to have a myelinated vagus, and this vagus nerve developed to synchronize the parasympathetic activity with these other forms of social engagement. The myelinated vagus converges with the other cranial nerves at the medulla, so these nerves can initiate similar, coordinated responses.6 For example, when someone feels secure, signals from the medulla in the brainstem will activate different cranial nerves to coordinate activity and maximize social engagement. Thus, the vagus nerve is an active player in the social engagement system.
Vagal Tone
A lot of cranial nerves are involved in the social engagement system, so you might be wondering what exactly the vagus nerve is doing in all of this. When the social engagement system is being used, the myelinated vagus nerve is active and promotes connectivity between the brain and the internal organs. Whereas most of the other cranial nerves relate to the muscles in the face and head, the vagus nerve is relaying these signals to internal organs we would not necessarily associate with social engagement. When the environment is perceived to be safe, the vagus nerve is sending signals to the body to promote parasympathetic activity (promoting rest and relaxation of bodily systems) and suppresses the sympathetic-adrenal system (mobilization of systems, i.e., fight or flight responses). This activity is referred to as vagal tone, which is defined as the amount of blood pumping from the vagus to the internal organs. When the system is engaged, the vagus is actively communicating to the body by sending blood, so vagal tone is high.
This process can be most easily observed at the heart. The heart has a natural pacemaker created by cells in the sinoatrial node. These cells cause the heart to rhythmically pump. However, this pacemaker is very fast (~110 beats/min)—much faster than our resting heart rate (~60-80 beats/min).8 Heart rate is regulated by inhibitory vagal tone, which slows the natural pacemaker so that the body is more relaxed. Because vagal tone slows the heartbeat, it is referred to as the vagal brake.1 Think of it like a car; regardless of how fast you pump the gas pedal, the car only accelerates after the brake is released. Vagal tone actually slows the heart such that we inhale quicker than we exhale, so we take in air quickly and then have time for it to circulate through our bodies before we release it. Therefore, our resting rhythm is considered arrhythmic and more variable. Vagal tone is correlated with heart rate variability, and we therefore often measure heart rate variability as a proxy for vagal tone.
Putting it Together
The vagus nerve is doing this when our body is in a resting state, or when no threat is perceived. Now let’s say that we perceive a threat. When a threat is detected, we engage the sympathetic system and inhibit the social engagement system. The myelinated vagus is less active, and the amount of vagal tone drops. Uninhibited, the heart beats more quickly and rhythmically; blood is quickly moving throughout your body to transport oxygen and sugar. This drop in vagal tone is also referred to as vagal suppression or the release of the vagal brake.
These stages of neural control are hierarchical. We actively use our myelinated vagus when possible, as it promotes a relaxed body state that uses little energy. Therefore, the myelinated vagus promotes prosocial behavior and low mobilization of resources, thereby promoting health and growth. When a threat is detected, resources are mobilized to the fight-or-flight responses rather than cortical processing (which is why you might have trouble remembering or thinking properly when you’re very stressed or nervous). The sympathetic-adrenal system is activated and, in extreme situations of stress, the immobilization response can be engaged.
By understanding the differences between these stages and when they are activated, we can deal with stress better and the negative health implications of chronic stress. It is natural to move between stages of the stress response, and these responses evolved to promote survival. However, it can be bad for your health to be constantly switching—it can negatively influence your health to have a stress response every day. Understanding the polyvagal theory can also help us to develop a better understanding of certain disorders. In the final post, I’ll discuss how polyvagal theory is used in research and clinical diagnoses.
References
1 Porges, S. W. (2009). The polyvagal theory: New insights into adaptive reactions of the autonomic nervous system. Cleveland Clinic Journal of Medicine,76(Suppl_2). doi:10.3949/ccjm.76.s2.17
2 Jardine, D. L. (2013). Vasovagal syncope: new physiologic insights. Cardiology clinics, 31(1), 75-87.
3 Drummond, P. D., & Lance, J. W. (1987). Facial flushing and sweating mediated by the sympathetic nervous system. Brain, 110(3), 793-803.
4https://www.resolvedhypnotherapy.co.uk/blushing-sweating-stammering/
5Porges, S. W. (2003). Social engagement and attachment. Annals of the New York Academy of Sciences, 1008(1), 31-47.
6Porges, S. W., Macellaio, M., Stanfill, S. D., McCue, K., Lewis, G. F., Harden, E. R., … & Heilman, K. J. (2013). Respiratory sinus arrhythmia and auditory processing in autism: Modifiable deficits of an integrated social engagement system?. International Journal of Psychophysiology, 88(3), 261-270.
7http://theweek.com/articles/458887/whats-point-baby-talk
8 Berntson, G. G., Quigley, K. S., & Lozano, D. (2007). Cardiovascular psychophysiology. Handbook of psychophysiology, 3, 182-210.